Top 5 Breakthroughs for Diabetes
Diabetes is one of the most pressing health issues in the world. According to the ADA (American Diabetes Association), close to 1.5 Americans are diagnosed with diabetes annually. Moreover, in 2017 the CDC (Centers for Disease Control and Prevention) reported that about 100 million people in the United States have prediabetes or diabetes.
One reason why diabetes remains one of the leading causes of death is poor nutrition, processed foods, and too much sugar. Although there’s no cure for diabetes, increased exercise and weight loss can help prevent Type 2 Diabetes.
With the advancements in medicine and technology, we are seeing tremendous improvement in preventing and treating diabetes. There are numerous types of research funded by many organizations such as the World Health Organization, related to finding innovative ways to treat and prevent diabetes.
-
A new way of preventing the immune system from attacking insulin-producing beta cells
One of the most exciting discoveries in healing diabetes as well as the field of medicine in general is a new way of preventing immune cells from attacking and killing beta cells that produce insulin. Immunotherapy treatment has been proven to be effective in decreasing immunosuppression.
Moreover, the treatment process can be customized for different individuals according to their specific medical state. The main reason why people with diabetes need to use medication is that the body’s ability to produce insulin become s impaired. According to Dr. song’s discovery, suppressing autoimmunity increases the chances of successfully treating Type 1 Diabetes.
-
Identifying what causes Type 1 Diabetes

Therefore, identifying exactly what causes the body to treat insulin-producing beta cells is a major leap towards finding treatment for Type 1 Diabetes. In recent years we have seen major advancement in this field where researchers are studying the possibility of avoiding suppression of the immune system by using immunoglobin to protect beta cells and hence increase insulin production.
-
Treatment of Diabetic Neuropathy
Patients suffering from neuropathy as a result of diabetes can experience nerve damage which can cause pain and other more serious diabetes-related complications such as sepsis. Neuropathy can also affect the spinal cord and brain.
Although diabetic neuropathy is very hard to treat, there is a new method of treating the condition where molecules are introduced to the body to prevent and potentially reverse neuropathy.
-
New Technologies for Diabetes
It is essential for diabetics to keep track of their blood glucose levels and blood pressure in order to effectively manage the condition by reacting faster.
Scientists have developed a new device that monitors glucose levels and automatically alerts the patient whenever their glucose levels fall below or rise above the target range. Moreover, we have seen great advancements in blood glucose monitors that have become more accurate, faster, smaller, lighter, and easier to carry around.
-
New Treatment for Type 2 Diabetes
In addition to the discoveries related to understanding what causes diabetes and finding ways to prevent the condition, there are new types of medication that will help diabetics by preventing side effects and other potential complications caused by diabetes.
Semaglutide, Liraglutide, and Glucagon are 3 new types of tablets that have been proven to be highly effective in the treatment of Type 2 Diabetes.
Semaglutide is a glucagon-based oral medication that should be used 30minutes before any beverage or meal. However, it is not recommended for use as an introductory treatment. In the first month, patients should take 3 mg and increase the dosage of Semaglutide to 7 mg after that.
Glucagon is a nasal powder that has been shown to be an excellent alternative to the injections most diabetes patients have been using. The good news is that it is available for all diabetics aged 4 years and above. However, it is essential to be aware of potential side effects of Semaglutide such as vomiting, headaches, and eye redness.
Liraglutide is recommended for type 2 Diabetes and is best for patients older than 10.
The Bottom line
One of the most important breakthroughs related to diabetes is related to numerous studies that have shown that the main cause of diabetes is poor nutrition and other lifestyle habits, especially among younger generations. Studies show that Type 2 Diabetes is mainly caused by processed foods, fast foods, too much sugar, and a sedentary lifestyle.
Therefore, the most effective way of preventing diabetes is by teaching the younger generation to increase physical activity and most importantly, adopt a healthier diet.





 Many diabetes support communities are created by diabetics and are safe places where people affected by the disease can learn from others, provide information, and seek advice from others without judgment, stigma, or fear. People with diabetes reap numerous tangible benefits from joining a Diabetes Online Community.
Many diabetes support communities are created by diabetics and are safe places where people affected by the disease can learn from others, provide information, and seek advice from others without judgment, stigma, or fear. People with diabetes reap numerous tangible benefits from joining a Diabetes Online Community. Diabetes chat rooms help diabetics create and join support networks that understand the nuances of managing diabetes on a deeper level. Therefore, they don’t feel alone.
Diabetes chat rooms help diabetics create and join support networks that understand the nuances of managing diabetes on a deeper level. Therefore, they don’t feel alone.
 According to the World Health Organization (WHO) and the Center for Disease Control and Prevention, SARS-CoV-2 is a virus that is common in animal species, and it rarely infects and spreads among humans. However, coronavirus first began infecting and spreading among humans in Wuhan, China in December 2019. From there, the disease has spread all over the globe.
According to the World Health Organization (WHO) and the Center for Disease Control and Prevention, SARS-CoV-2 is a virus that is common in animal species, and it rarely infects and spreads among humans. However, coronavirus first began infecting and spreading among humans in Wuhan, China in December 2019. From there, the disease has spread all over the globe.
 The exact cause of diabetic myopathy is not fully understood. However, it is believed to be a result of long-term high blood sugar levels. High blood sugar levels can damage the blood vessels that supply the muscles with oxygen and nutrients. This damage can lead to muscle weakness, wasting, and pain.
The exact cause of diabetic myopathy is not fully understood. However, it is believed to be a result of long-term high blood sugar levels. High blood sugar levels can damage the blood vessels that supply the muscles with oxygen and nutrients. This damage can lead to muscle weakness, wasting, and pain.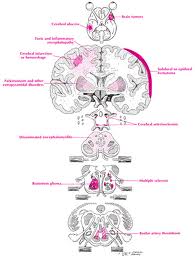 The symptoms of diabetic myopathy can vary from person to person. However, some common symptoms include:
The symptoms of diabetic myopathy can vary from person to person. However, some common symptoms include: