6 Tips for Diabetes Foot Care
What is proper foot care for diabetics?
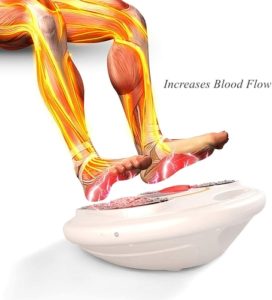
People with diabetes are more likely to suffer from neuropathy and other foot problems as a result of nerve damage and reduced blood flow to the feet. Small sores and cuts may also take longer to heal. The biggest risk is infection when germs get into cracks or cuts.
Poor foot care with diabetes can lead to foot or leg amputation. Therefore, if you have an infection, it is essential to seek medical attention right away to keep it from spreading and causing other complications.
According to the ADA (American Diabetes Association), 1 in 5 diabetes patients seek medical care due to foot problems. Fortunately, you can avoid foot problems by keeping your blood glucose levels within the recommended range.
Here are some preventive measures diabetes patients can take to keep their feet healthy:
1. Wash your feet daily and keep them dry
Make it a daily ritual to wash your feet in warm water using mild soap to ensure that areas that are prone to infection remain clean and free of debris and dirt. Avoid using hot water and soaking your feet for too long as this could easily damage your skin. Use a sponge or soft cloth to wash your feet and dry them thoroughly after your foot bath.
Remember not to leave any moisture between the toes as this could break down the skin or cause fungus to grow leading to infection. Apply moisture to any cracked areas and away from your toes to avoid infection. Apply non-medicated powder before wearing socks and shoes to keep your feet dry.
In winter, central heating can help keep your feet dry and warm. Be sure to wear socks in cold weather or whenever your feet get cold.
2. Check your feet regularly
Doctors recommend checking the bottoms and tops of your feet daily. You can request someone else to do it or use a mirror if you can’t see them. Look carefully in good light so you can see problems such as cracked skin on the heels, toes, and feet.
Check your heels, feet and toes for cuts, blisters, scrapes, bruises, scratches, and other sores. Look between the toes for fungus and cuts that may cause infections or athlete’s foot.
Check for tenderness, redness, increased warmth, corns, calluses, and ingrown toe nails. Avoid “popping” blisters caused by your shoes. Put bandages over them and wear comfortable shoes.
3. Diabetic toenails – take care of your toes

You may want a foot doctor (podiatrist) or nail technician to trim your toenails for you. If you visit a nail salon for pedicures, bring your own tools. Avoid cutting cuticles and don’t use sharp tools to remove calluses or to clean under the toenails. This will help you prevent accidental cuts that could lead to infection. A pumice stone is great for smoothing the heels after washing your feet or taking a bath or shower. Be sure to rub gently to prevent injuries.
4. Be careful when working out
It is essential to work out regularly to maintain healthy blood flow. Workout for at least 30 minutes daily and be sure to do it in fitting, comfortable shoes.
Ask your physician what type of physical activities you should engage in if you have open injuries on your feet.
5. Avoid going barefoot
Don’t go only in socks or barefoot to avoid stepping on tacks, rocks, and other objects that could injure your feet. Protect your feet with hard-soled slippers, shoes, or similar footwear. Always protect your feet from moisture and cold. You can wear flip-flops at home.
Avoid wearing shoes with pointed toes and high heels or shoes that leave your heels or toes exposed, like slippers, open-toed shoes, and sandals. Wearing such footwear outdoors leaves your feet exposed to injury which could lead to infections.
Wear neutral materials such as wool, cotton, or cotton-wool blends. Don’t wear tight socks or socks with materials or rough areas that rub against the skin. Avoid tight-fitting shoes and look inside your footwear before wearing them to make sure there are no rough areas or irritating objects in them. Replace shoes that are showing signs of wear, and wear the type of shoes recommended by your doctor.
6. Wear fitting, comfortable shoes
Is your shoe too narrow? Are your feet crammed into your shoes? If you have nerve damage (neuropathy) it could be hard for you to notice that your footwear is too tight.
Your shoes should be as wide as your feet and about ½ inch longer than the longest toe. Shows that are too loose or too tight may cause injuries, such as blisters.
If you have diabetes, shop for shoes that have:
- Outer soles made of stiff materials
- Closed heels and toes
- Leather upper without suede, canvas, or seams inside. Choose shoes with cushioned soles to absorb pressure. It is also essential to note that shoes with laces provide better support compared to loafers.
- Soft insides without any rough areas
Avoid wearing new shoes for extended durations. Break in them slowly by wearing them for 1 or 2 hours a day.
Although well-fitting shoes are extremely important, you may also want to consider wearing diabetic socks to keep your feet injury-free and healthy. Diabetic socks can help keep your feet warm and dry, improve blood flow, provide cushion, and prevent fungal infections.
When you buy through links on our website, we may earn a small commission at no cost to you. Thanks for your support 🙂
The best diabetic socks have features such as:
- Stretchy cuffs to promote blood flow
- No seams and rough materials to prevent rubbing
- Moisture-wicking materials that help keep your feet dry
- Soft and thick at the ball and heel of your foot
- Comfortable fit with no bunches or wrinkles
The bottom-line
If you have any injuries on your feet, be sure to seek medical attention and follow your doctor’s recommendations and guidelines. Don’t self-treat foot problems such as calluses, scratches, blisters, cuts, scrapes or corns.
Check water temperature using a thermometer or your elbow, not your feet. Seek medical attention if you notice foot problems such as cracking between toes (athlete’s foot), ingrown toenails, increasing pain or numbness, signs of infection (redness, drainage, or swelling), bunions, blackening of the skin, hammertoes (bent middle joints), and nails that seem changed in shape, striped, yellow, or thicker.




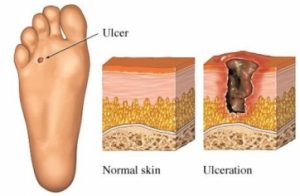 Diabetic foot sores and infections are common complications of poorly managed or unmanaged diabetes. Diabetes is managed through various methods including insulin treatment, exercise, and diet.
Diabetic foot sores and infections are common complications of poorly managed or unmanaged diabetes. Diabetes is managed through various methods including insulin treatment, exercise, and diet.



 The most complex
The most complex 

 According to the World Health Organization (WHO) and the Center for Disease Control and Prevention, SARS-CoV-2 is a virus that is common in animal species, and it rarely infects and spreads among humans. However, coronavirus first began infecting and spreading among humans in Wuhan, China in December 2019. From there, the disease has spread all over the globe.
According to the World Health Organization (WHO) and the Center for Disease Control and Prevention, SARS-CoV-2 is a virus that is common in animal species, and it rarely infects and spreads among humans. However, coronavirus first began infecting and spreading among humans in Wuhan, China in December 2019. From there, the disease has spread all over the globe.