What is a Diabetic Foot Ulcer?
A foot ulcer forms when skin tissue anywhere on the foot or toes breaks down exposing inner layers. It can involve the entire thickness of your skin, including deep structures such as tendons or bones. On the other hand, it can be redness or a shallow sore that involves only the skin surface.
People with poor circulation and diabetes patients in particular, are at a higher risk of developing foot ulcers. In people with diabetes, foot ulcers can be difficult largely because even small foot ulcers can easily become infected, especially if it is not treated properly.
Sometimes you may not know you have foot ulcers until you notice wetness or drainage on some parts of your socks. Drainage can be red, brown, or yellow and it may also contain blood or pus.
If a foot ulcer becomes infected and if not treated promptly, it can gradually develop into:
- A pocket of pus (an abscess)
- Cellulitis (a spreading infection of underlying fat as well as the skin)
- Osteomyelitis (a bone infection)
- Gangrene (an area of dead body tissue as a result of poor blood flow)
In uncontrolled or poorly controlled diabetes severe foot infections may eventually require some part of the lower leg, foot or toe to be amputated usually start as a foot ulcer.
Factors that Increase the Risk of Diabetic Foot Ulcers
- Poor blood flow

- Numbness and nerve damage in the feet
- Uncontrolled blood sugar levels
- Corns or calluses on your toes or feet
- Foot deformities such as hammertoe or bunion
- Poor vision that causes you to trip on objects in your way
- Alcohol use or cigarette smoking
- Being overweight
Diabetic Foot Ulcer Treatment Options
-
Antibiotic cream for foot ulcers
Your diabetic healthcare provider may suggest applying antibiotic cream to help prevent infection and relieve the sore. Thereafter, it’s important to cover the area to avoid infection or further damage.
-
Wound dressing of foot ulcers
A bandage or other types of dressing will be put on the ulcer and your doctor will give you instructions in the changing routine. The dressing may contain medication to help the ulcer heal faster and prevent growth of unhealthy tissue. If the sore is already infected, your doctor will give you antibiotics to fight the infection.
-
Have dead tissue removed (debrided)
Removal of any dead tissue and skin around foot ulcers can help with healing and prevent infection.
-
Manage your blood glucose levels and any other health problems
Health issues such as blood sugar levels, cholesterol and blood pressure need to be managed to help foot ulcers heal. Your doctor will help you create a plan to manage any health issues you may have.
-
Take the pressure off your foot ulcer
In some cases, you may need special support shoes with braces, cushions, or insoles to offload the pressure off your foot ulcer. You may also be advised to use crutches or a wheelchair until your foot ulcers heal. These items help keep irritation and pressure off the area of the foot ulcer. Foot ulcers heal faster without irritation and pressure.
-
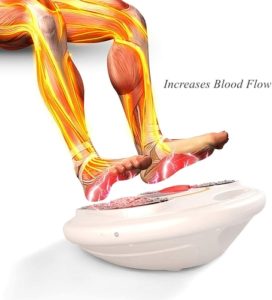
Increase blood flow to your feet
 Your doctor may recommend negative pressure wound therapy or hyperbaric oxygen therapy to increase blood flow to the lower extremities. You can consult your healthcare provider for more information about these treatment techniques.
Your doctor may recommend negative pressure wound therapy or hyperbaric oxygen therapy to increase blood flow to the lower extremities. You can consult your healthcare provider for more information about these treatment techniques.
-
Visit a specialist as directed
Your doctor may advise you to see a vascular surgeon, an orthopedic, or a podiatrist. These professionals can help you manage your specific condition and treatment regimen.
-
Negative pressure wound therapy
This diabetic foot ulcer treatment option involves the use of a vacuum to remove extracellular waste and fluid from the wound. The administration of negative pressure wound therapy requires specialized skills for positive outcomes in treating wounds and ulcers.
-
Extracellular matrix replacement therapy
A diabetic foot ulcer is primarily a complication of Type 2 Diabetes that needs timely intervention to avoid more serious outcomes such as amputation. Research shows that diabetic foot ulcers are responsible for about 84 percent of all lower leg amputations. Diabetic foot ulcers are considered to be a result of micro and macrovascular complications.
Slow healing or failure of sores and wounds to heal as a result of chronic diabetes can be treated with extracellular matrix replacement therapy. Diabetes foot ulcer treatment largely rests on techniques such as negative pressure wound therapy, skin substitute, and advanced moist wound therapy.
When it comes to treatment for foot ulcers, you should keep in mind that different treatment options and therapies have different benefits and side effects as well. Moreover, diabetic foot ulcer treatment can vary depending on the causes. Therefore, it’s important to discuss different options with your healthcare provider to determine the most suited therapy or treatment option.

