Who Needs a Gestational Diabetes Meal Plan?
Statistics have shown that roughly five percent of pregnant women may develop gestational diabetes, a condition in which a woman who doesn’t suffer from diabetes, suddenly becomes diabetic during and usually in the second half of her pregnancy.
When something like this happens, blood sugar monitoring should be done regularly to avoid any complications that may arise during labor.
How Effective is a Gestational Diabetes Meal Plan?
When a woman develops mild gestational diabetes, it is important that a proper diabetic meal plan is implemented with the help of a professional nutritionist to help control blood sugar levels. If the diabetes is allowed to progress into a stronger condition, insulin therapy may need to be introduced to help lower blood sugar levels.
How do you Design a Great Gestational Diabetes Meal Plan?

Because it’s not only you that is being affected by Gestational diabetes, but also your unborn baby, you should really seek out professional help to make sure that you are both getting all of the nutrients you need, while keeping your blood sugar levels in check at the same time.
Gestational Diabetes Symptoms
A good majority of the time, there are no symptoms, or very mild. These can include:
- Weight loss – even though you are eating more!
- Blurred vision
- Nausea and vomiting
- Increased thirst and Urination
- Increased infections, particularly of the bladder and vagina.
- Fatigue
- Raised blood sugar, which will generally stabilize after the birth
Causes of Gestational Diabetes.
- If you are carrying extra weight prior to becoming pregnant
- If you have a family history of Diabetes Type 2
- If you fall into the category of ‘Pre-Diabetes’ which is raised Blood Sugar, but not high enough to be classed ‘Diabetic’ (Read More about Pre-Diabetes)
- Women over the age of 25 are more at risk.
- If you have previously given birth to a baby that weighed more than 9 pounds.
- If you have Polycystic Ovary Syndrome.
- If you are a Pacific Islander, Hispanic, African American or American Indian.
- You have given birth to a stillborn baby in the past.
A Sample Diabetes Meal Plan
If you are brainstorming for ideas for the meal plan, here are some tips:
Breakfast
Get yourself some starchy vegetables along with whole wheat bread, drink some milk to get a good intake of protein. If you want, you may also add a bagel spread with a teaspoon of jam.
Lunch
You can grab a sandwich made with whole wheat bread with two ounces of protein-rich meat, such as roasted turkey, lean roast beef, or fresh tuna. You can use a tablespoon of salad dressing or mayonnaise along with your sandwich for flavor. Finally, add a cup of nonfat yogurt or some milk to get your dairy requirement for this meal.
You may want to get more protein and having some grilled chicken or salmon (approximately three ounces) would be a great start. Next, you’ll want to get your carbohydrate of choice, with suggestions of either a cup of pasta or large baked potato and to this add a cup of steamed asparagus or some tossed salad with low-fat salad dressing.
Lastly, for dessert, you can enjoy a cup of fresh apricots, melons, or other fruit.
Snacks!
If you feel hungry, you may want to get some snacks like whole wheat crackers or tortilla chips to help tide you over between meals. If you choose to go this route, just remember to keep the snacks small, so that your gestational diabetes meal plan is effective while at the same time enjoyable!



 Even the calmest of Mothers-to-be will become concerned if they are diagnosed with gestational diabetes. It’s a sad fact that more and more women are going to receive this worrying news as gestational diabetes is on the rise.
Even the calmest of Mothers-to-be will become concerned if they are diagnosed with gestational diabetes. It’s a sad fact that more and more women are going to receive this worrying news as gestational diabetes is on the rise. During pregnancy, the placenta is responsible for providing nourishment to the baby from the mother. Hormones released by the placenta cause a slight insulin resistant state in the mother as a normal part of pregnancy. As insulin is important for moving sugars into the cells, it plays an integral roll in maintaining steady blood sugar levels.
During pregnancy, the placenta is responsible for providing nourishment to the baby from the mother. Hormones released by the placenta cause a slight insulin resistant state in the mother as a normal part of pregnancy. As insulin is important for moving sugars into the cells, it plays an integral roll in maintaining steady blood sugar levels.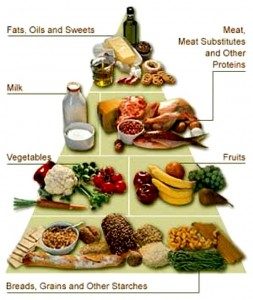 A healthy diet is essential in pregnant women diagnosed with gestational diabetes. Reducing carbohydrates to 40 or 45per cent of your diet while making sure any carbohydrates have a low glycaemic index (GI) and low glycaemic load is crucial.
A healthy diet is essential in pregnant women diagnosed with gestational diabetes. Reducing carbohydrates to 40 or 45per cent of your diet while making sure any carbohydrates have a low glycaemic index (GI) and low glycaemic load is crucial.