What is Juvenile Diabetes?
Read about the Causes, Signs, and Symptoms of Juvenile Diabetes.
Being diagnosed with any condition or disease can be very scary, especially when it happens to our children. Will the disease affect their ability to lead a normal teenage life? Will they struggle even more when they become adults? In the case of Type 1 Diabetes, which is also referred to as juvenile diabetes, the important and good news is that the condition is totally manageable. Here are some of the things you need to know about the symptoms, causes, risk factors, and treatment of juvenile diabetes.
What is Juvenile Diabetes?
Juvenile diabetes (Type 1 Diabetes) is an autoimmune disorder that is usually diagnosed in adolescence or childhood but can also occur in adults aged between 30 and 40 years. It’s a chronic condition in which the pancreas makes little or no insulin and as a result, sugar starts building up in the bloodstream, which can cause a wide range of life-threatening complications. Therefore, people with Type 1 diabetes must take insulin in order to prevent complications and live healthy lives.

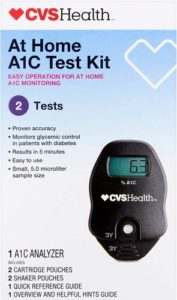
Despite active scientific research, juvenile diabetes has no cure and treatment mainly focuses on diet and lifestyle and managing blood glucose levels using insulin to prevent complications.
According to recent studies, about 193,000 children and adolescents have diabetes; about 77 percent of those cases are Type 1 Diabetes (juvenile diabetes).
How Does Glucose Work?
After eating, the body breaks down food into various substances including glucose, which is then absorbed into the bloodstream. The pancreas is mainly responsible for producing insulin, which helps fat cells and muscles absorb glucose (sugar) and use it for energy.
In people with juvenile diabetes, the immune system attacks the beta cells that make insulin, reducing or stopping production. With little or no insulin to help cells absorb glucose, sugar builds up in the blood, leading to various health issues.
What a the Common Causes of Juvenile Diabetes?
Researchers don’t know exactly what causes juvenile diabetes because it’s not linked to any specific gene that can be tested for. Although some autoimmune disorders tend to run in families, a large number of juvenile diabetes cases happen randomly. According to studies, some of the possible factors that contribute to the development of the condition include:
- Geography and ethnicity: Juvenile is more common among people who live further away from the equator. Research shows that children and adolescents in Scandinavian countries generally have a higher risk of developing the condition. Caucasians of Northern Europe ancestry also have a higher risk of being diagnosed with the disease than other ethnicities.
- Infections and toxins: Researchers believe that in a large number of cases a virus or toxin triggers the start of juvenile diabetes by triggering the immune system to mistakenly attack beta cells in the pancreas.
- Family history: Children from families with a history of autoimmune conditions are at a higher risk of being diagnosed with Type 1 Diabetes. If a parent or sibling has juvenile diabetes, children are 15 times more likely of being diagnosed with the disease than people without a family history of autoimmune diseases.
- Genetics: While there’s no specific Type 1 Diabetes gene, there are some mutations and genes that have been linked to an increased risk of developing Type 1 Diabetes. For instance, mutations in HLA (Human Leukocyte Antigen) class of genes can increase the risk of various autoimmune conditions, including juvenile diabetes.
What are the Symptoms of Juvenile Diabetes?
Although having these symptoms does not automatically mean your kid has juvenile diabetes, it’s critical to consult their pediatrician if you notice one or more of these symptoms.
- Extreme thirst: Too much glucose in the bloodstream triggers the body to pull water from surrounding fat cells and tissue to dilute it. This makes some kids extremely thirsty and dehydrated. Kids with diabetes may feel that no matter how much water (and other fluids) they drink, their thirst can’t be quenched.
- Frequent urination or having pee accidents: In a bid to reduce sugar in the bloodstream, the kidneys filter it and try to dump it into the urine. As a result, more pee is created and the need to urinate increases. Children with juvenile diabetes may start having frequent pee accidents both at night and during the day, despite having been potty-trained. Some kids with juvenile diabetes may feel the urge to urinate frequently. The risk of UTIs (urinary tract infections) is also higher in kids with juvenile diabetes.
- Dry mouth and bad breath: When the body starts breaking stored fat for fuel, the process creates chemicals known as ketones that may cause children to have bad breath (stale smell). The same thing tends to happen to people who go on low-carb diets.
- Weight loss: For children who are eating normally and are otherwise healthy, sudden weight loss could be a symptom of juvenile diabetes. This usually happens when the cells are not getting the glucose they need out of the bloodstream. As a result, they start breaking down muscles and storing fat for energy instead.
- Fatigue and general weakness: Kids with juvenile diabetes may feel weak and tired because their body systems including the brain and muscles are not getting the energy they need to function optimally. Fatigue can also be a result of dehydration from peeing frequently. Sometimes, weakness and listlessness can be a sign of serious complications such as ketoacidosis, which can be deadly and requires immediate attention.
- Vomiting, belly pain, confusion, and fainting: Ketoacidosis can cause vomiting, and severe stomach aches, and usually causes kids and young adults to lose consciousness or act confused.
What are the signs of an emergency with juvenile diabetes?
- Belly pain
- Fruity smell to the child’s breath
- Confusion and shaking
- Loss of consciousness (rare)
- Rapid Breathing
Managing juvenile diabetes can be challenging for both parents and their kids. However, the growing number of support systems and treatments for people with the disease has made it easier than ever to live a happy normal life.
Read more about the signs and symptoms of diabetes in toddlers HERE!






 Your dogs’ vet will examine your dog and determine the number of calories they need per day, depending on their activity level and weight. Once you know how many calories your pooch needs, it is vital to closely monitor what they consume and how much.
Your dogs’ vet will examine your dog and determine the number of calories they need per day, depending on their activity level and weight. Once you know how many calories your pooch needs, it is vital to closely monitor what they consume and how much.

 Several hundred islet cell transplants have already taken place and the success rate of the procedure has been steadily improving and could soon rival kidney transplantation’s success rate!
Several hundred islet cell transplants have already taken place and the success rate of the procedure has been steadily improving and could soon rival kidney transplantation’s success rate!