Complications of Diabetes
What are the Main Diabetic Complications to be Aware of?
If blood glucose levels become elevated and stay high for a long period of time, some parts of the body may become progressively damaged. This damage is not inevitable – most people with diabetes stay healthy and free from complications. This article will show you why diabetic complications are worth preventing and what you can do about they if they do occur.
Your Heart.
The body depends on the flow of blood for it’s survival. If blood flow is stopped even for a brief period, cells and tissues downstream from the blockage will suffer and may even die. When this occurs in the heart, it is called a heart attack or myocardial infarction. When this occurs in the brain, it is called a stroke.
Together, heart attacks and strokes are the most important complications of diabetes type 2. They are also among the most preventable. There are several ways you can prevent them from happening to you.
Blood Pressure.
Blood pressure is the force generated by the heart as it pumps blood through your body. The systolic blood pressure is your beating heart’s maximum pressure, which you feel as your pulse. It is also the major stress on the surface of your blood vessels. Diabetes makes the blood vessels stiffer and less able to relax, increasing the pressure inside them.
This condition is called hypertension in diabetics. If you have diabetes, you should have your blood pressure checked every time you visit your doctor. Reducing your systolic blood pressure will in turn reduce your long-term risk of heart attack or stroke. Most people can achieve this through a combination of diet, regular exercise and appropriate medication. Relaxation therapy, yoga and medication can also lower blood pressure.
There are several ways to reduce your Blood Pressure:
Lose Weight: For every kilogram of weight you lose, your systolic blood pressure goes down on average by about 1 mmHg
Exercise Regularly: This can lower your blood pressure by as much as 10 mmHg. If your blood pressure is normal, exercise can also prevent if rising as you age. For your exercise program to reduce your blood pressure, it must include aerobic activity such as brisk walking, climbing stairs, jogging, bicycling or swimming. Try to include at least 30 minutes of aerobic exercise on all or most days of the week.
Reduce your salt intake: This will not only lower your blood pressure but also make your blood-pressure medications more effective. If you have diabetes, you should try to reduce your salt intake to less than 4 grams a day. More than 75% of the salt in the average diet is hidden in processed foods such as bread, cereals, cheese, soups, sauces, stock powder and condiments. Look for alternatives and products labelled as reduced-salt, no added salt or low salt. Use herbs and spices instead of salt to add flavour to your food.
Eat more fruit and vegetables: diets high in fruit and vegetables can also help reduce blood pressure. Try to include two serves of fruit and 5 serves of vegetables in your diet every day. One way to do this is to follow our diabetes eating plan.
Eat more fish and omega 3 oils: Including oily fish in your weight loss diet can help reduce blood pressure more effectively than weight loss alone. Fish oil supplements can also reduce blood pressure, but you need to take them regularly and in large amounts (eg 4 grams a day)
Limit your alcohol intake: There is an established link between excessive alcohol and hypertension. Limit your alcohol intake to no more than 2 standard drinks each day for men and 1 standard drink each day for women.
Giving up Smoking.
Smoking significantly increases your risk of heart attack and stroke. Toxins in cigarette smoke damage the surface of blood vessels and even passive smoking puts you heart at risk, so encourage others to stop too. Talk to your doctor to find out the best options for you. If you quit for good, you can reverse some of the damage caused by smoking. If you can keep off the cigarettes for more than a decade, your risk of heart attack and stroke will be almost as that of a non-smoker.
Controlling your blood glucose levels.
A high blood glucose level means you are at the highest risk of heart attack or stroke. Any effort to better control your glucose levels will significantly reduce your heart attack risk.
Diabetes and the Eyes.

To form and image in your brain, light must pass through the iris, be focused by the lens reach your retina and pass as an electric signal down the optic nerve. Diabetes can disrupt any or all parts of this pathway. Reducing the quality of the picture or blocking part of the image. Diabetes is especially damaging to the small blood vessels at the back of the eye, which can result in a number of complications including the following:
Macular Oedema: The macula sits at the centre of the retina and is responsible for seeing fine details. If diabetes damages the blood vessels near the macula, they can leak fluid, causing the retina to swell (which is know as oedema) and your vision to be reduced.
Retinal ischaemia: Damaged blood vessels can sometimes become blocked, reducing the supply of oxygen and nutrients to parts of the retina and reducing vision.
Proliferative Retinopathy: Diabetes sometimes triggers a proliferation of new blood vessels in the eye to take the place of damaged ones. But far from being helpful, these new vessels can promote scarring ad more damage. They are very fragile and prone to spontaneous bleeding. As scar tissue associated with the new vessels shrinks, it can also sometimes pull the retina right off, leading to permanent loss of vision in the detached area.
Cataracts: Diabetes can cause the lens of your eye to become clouded. Nearsightedness is an early sign of cataracts. Cataracts also scatter the light entering the eye, making things appear less vivid with less contrast, especially in low light. People with cataracts may also experience glare with bright lights, such as car lights. Eventually, cataracts can obstruct the passage of light into the eye and reduce vision. Many of us will experience a degree of vision loss due to cataracts as we age, but diabetes makes it more likely and may cause it to occur at a younger age.
Preventing Eye Damage
Although eye damage is very common in people with diabetes, it is often possible to prevent significant vision loss or blindness through the following:
Do Diabetics need Regular Eye Tests :
Get your eyes examined regularly – once a year preferably, by an optometrist or ophthalmologist, even if your vision is normal. In diabetes, the damage to the eyes is insidious, with no pain and few symptoms. If you notice problems with your vision, it may be too late. If you already have early signs of eye damage, high blood pressure or kidney disease, you will need to have your eyes examined more frequently.
Don’t Ignore Symptoms:
Rapidly report any sudden changes in your vision to your doctor or eye specialist. Treatments are most effective when damage is caught in the early stages.
Control Your Diabetes:
Maintain good control of your glucose, lipid and blood-pressure levels.
Protect Your Eyes:
Avoid exposure to the ultra violet and infrared rays in sunlight, which can contribute to cataract development. Wear UVB-protecting sunglasses and a broad brimmed hat, and avoid direct sunlight in the middle of the day.
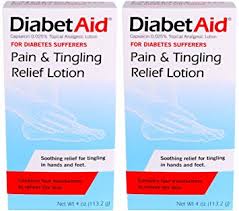
Looking After your Feet
Diabetes and Feet: Your feet are especially vulnerable to Diabetes. It can damage the nerves in your feet (know as neuropathy) which can make them numb to injuries or damaging pressure. Nerve damage can also sometimes be painful, producing pins and needs or a burning sensation, which is often worse at night. Damage to the nerves also makes the muscles in the feet weak or uncoordinated, which can cause foot deformities, such as bunions or hammertoe. These increase the stresses on your feet and can lead to corns, calluses, blisters and ulcers.
Diabetes can also damage the blood vessels that supply the feet, reducing the flow of blood, oxygen and sustaining nutrients to the furthest reaches of your body. High glucose levels also impair your ability to fight off infections that get under your skin through cracks or ulcers in your feet or into your toenails. If left untreated, these infections can spread and kill of tissues in your feet (known as gangrene). Diabetes can also alter the skin on your feet, making it thicker, drier, less resilient and more prone to blisters or cracks (especially at the heel).
Preventing Foot Damage : There are many simple steps you can take to avoid damage to your feet.
- Pay attention to them. Inspect your feet every day for early signs of trouble or potential problem areas. Use a hand mirror to see the entire bottom of your feet and check between your toes. Before you put your shoes on ,check them for stones, sticks and other foreign objects that might hurt your feet. Take off your shoes and socks every time you see your doctor.. Your feet should be examined by a doctor or podiatrist every three or four months.If you already have signs of foot problems you must have regular podiatry care.
- Look after your toenails. Many foot problems begin in and around the toenails. Thickened nails or sharp edges that dig in (without you feeling them) are often the opportunity an infection needs to get started. Keep your toenails trimmed straight across following the curve of your toes and file the edges with an emery board or nail file. Have a podiatrist do this if you need help or are unsure, or can’t see or reach your toes well.
- Keep the skin on your feet healthy. Wash and dry your feet very well every day, but don’t soak your feet or put them in very hot water. Moisturize dry areas, such as the heel, with lotions that don’t contain alcohol. Keep moist areas, such as between the toes, dry.
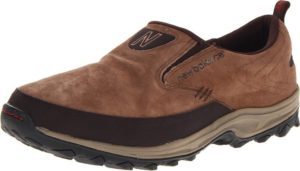
- Buy good shoes and socks. Many ulcers come from poorly fitting shoes or or going barefoot unnecessarily. Always wear shoes properly fitted to the shape of your feet. Specialty shoe shops are usually better equipped than discount or department stores. If they don’t know about diabetes, go somewhere else where they do. Choose shoes that give more room to your toes with thick cushioning rubber soles but never high heels. Special shoes with extra cushioning or orthotics can be useful if you are at increased risk of foot problems. The right socks are also important in keeping your skin dry and cool. These are usually acrylic, not tight and don’t have seams. Some also have special cushioning. Always wear clean socks and throw out damaged, tight or old ones.
- Don’t add to your risk. Maintaining good control of your glucose, cholesterol, lipids and blood-pressure levels is an important way to prevent foot damage. Smoking – even passive smoking increases the risk or needing an amputation.
- Don’t ignore foot problems. Immediately report andy changes in your feet to your doctor or foot specialist. Don’t ignore them and hope they go away. The earlier you detect an infection, the better the chance of doing something about it. Important warning signs include: Redness or skin discoloration, especially around corns or calluses: Swelling or changes in the size or shape of your feet or ankles : Pain in the feet or legs at rest or while walking (even if you feel no pain, there could still be cause for concern.): blisters : bleeding : open sores (ulcers), no matter how small : and hot or cold spots. There are a number of effective treatments that can help your feet to heal. These can include : Cleaning and dressing the wound : staying off damaged feet: antibiotics to help the infection heal and prevent it from spreading: and surgery, which is sometimes necessary to help ulcers heal.
Your Mood
Staying Healthy is about more than just keeping your glucose levels down. You also need to maintain and optimise your mental well being.
Diabetes and Depression:
Depression is not just a brief period of feeling low, but a disproportionate and pervasive mood that interferes with your ability to function. It can affect your relationships, work, sleep and many other aspects of health and well being. Depression can also affect your diabetes control, the likelihood of complications and their impact.
Adults with diabetes are more likely to develop depression or other forms of mental illness than people without diabetes. Various factors can contribute to the development of depression, including the following:
- The guilt and perceived stigma associated with having diabetes.
- The stress of living with diabetes and the demands of managing it successfully.
- Chronic pain or disability associated with diabetic complications.
- Low physical activity
- A strong family history of diabetes and exposure to it’s consequences.
- Changes in the balance of chemicals in the brain caused by diabetes.
- Damage to the small blood vessels in the brain that regulate brain function.
- Increased levels of inflammation, associated with diabetes, triggering the release of cytokines, signalling molecules that modify brain function.
- Insomnia, especially for sufferers of obstructive sleep apnoea.
- Certain medications, such as beta blockers.
Preventing Depression:
Not everyone who has diabetes will become depressed. Simply looking after your diabetes will help reduce your risk of depression. The more competent you become at looking after yourself, the lower will be your stress and risk of depression.
Where possible, enlist the support of your diabetes care team, family and friends. Support groups can also help reduce the risk of depression. Find out about local diabetes meetings or consider joining one of the many diabetes organizations.
Treating depression:
Depression is not something you have to put up with – it can be treated. The effective treatment of depression will also mean better diabetes control and reduced risk of complications. A number of different treatment options are available, including the following. Your doctor witll decide which, alone or in combination, will work best for you.
Your Sleep
Without sleep we don’t only feel tired, but our bodies don’t work as well. Inadequate sleep can lead to weight gain and makes it harder to control blood pressure, cholesterol and glucose levels. Poor sleep is actually associated with an increased risk of diabetes. Sleep also affects your mood, sensitivity to pain and resistance to infection.
Diabetes and Sleep:
Diabetes can have an impact on your nights as much as your days. Diabetes can stop you getting the sleep you need by causing:
- A need to get up at night to use the bathroom
- Shortness of breath when lying down
- Restless legs and cramping
- Painful feet (due to ulcers, infection, nerve damage or vascular disease)
- Stress or depression
- Obstructive sleep apnea